
By Professor Noel Fitzpatrick
Managing DirectorFitzpatrick Referrals is passionate about understanding the evolution of small animal diseases and working in tandem with specialists across the human medical field.
These unique collaborations have allowed us to become the only centre in the world offering some surgical treatments for companion animal diseases which include custom-made partial and total replacements for the shoulder, elbow, stifle and tarsocrural joints in dogs affected by severe lameness.
Elbow dysplasia, which is now more properly termed developmental elbow disease, is one of the most common causes of forelimb lameness in young, large and giant breed dogs. We asked the orthopaedics team some of your frequently asked questions about canine developmental elbow disease and the treatment options available at Fitzpatrick Referrals.
1. What are the symptoms of developmental elbow disease (DED)?
Lameness can sometimes be noticed by a nodding head; a dog will lift their head when the lame forelimb is placed so as to transfer weight to their hindlimbs and other forelimb to reduce impact on their painful joint/s. Dogs that are bilaterally lame may have an unusual ’paddling’ gait. Lameness is often triggered by prolonged rest and sudden exercise. For this reason, many dogs will be lame when they wake up but after a warm-up, they will exercise freely and then be lame again afterwards. Although most dogs will be diagnosed before they are two years old, some dogs will not become lame until they are older or lameness may not be noticed if it is bilateral. DED is more common in medium and large breed dogs, but small breed dogs can also be affected, and DED should be considered a differential in any dog with forelimb lameness that has not been caused by trauma.
2. How do you diagnose DED?
In a primary care setting, we would recommend a full orthopaedic clinical examination of the forelimbs to isolate definitive pain associated with elbow manipulation, followed by mediolateral and cranio-caudal radiographic projections of both elbows under deep sedation. This should allow a moderately confident diagnosis of DED or subsequent osteoarthritis. If you are unsure, radiographs can be submitted to our radiographic opinion service free of charge.
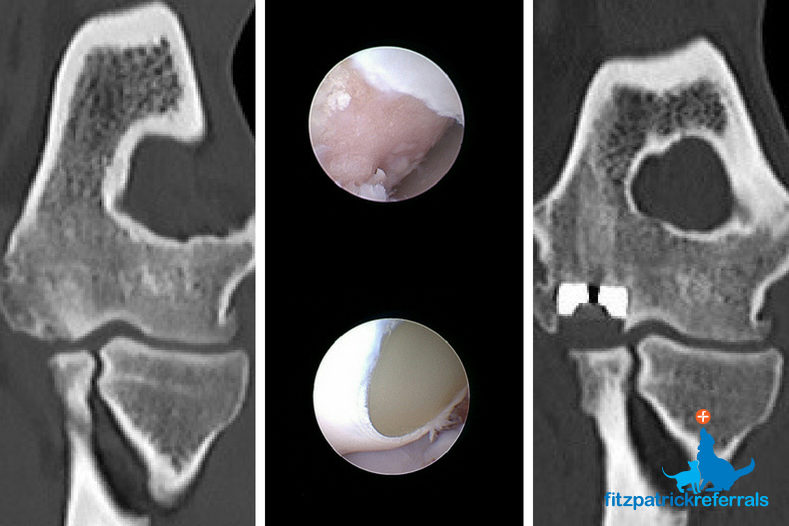
Once referred, a full orthopaedic examination will be repeated followed by a CT scan using our Toshiba Aquilion 160 slice CT scanner which provides excellent image quality within seconds of scanning time. Although radiographs will usually show changes in the elbows of dogs affected by DED and osteoarthritis, this is not always the case because at times changes can be very subtle and difficult to detect. CT scans help to confirm a diagnosis of DED, give more information about the extent of disease and allow our specialists to decide what interventions would be most helpful for each individual dog and family, whether they be surgical, medical, regenerative or a combination. The majority of dogs will also have arthroscopy as part of the investigation process and to further guide the most efficacious intervention. Arthroscopy allows us to directly observe the cartilage, bone and synovial tissue inside the joint.
3. What is DED?
Disease conditions encompassed by the syndrome of DED include medial coronoid disease (MCD) which may progress to medial compartment disease (MCompD) due to humero-ulnar conflict and elbow Incongruity (EI). This is characterised by fissuring or fragmentation of the medial coronoid process and often progressive cartilage erosion of the medial compartment. Fissuring is graded arthroscopically according to location and cartilage erosion is graded 0-5 (modified Outerbridge score) with 5 being full thickness raw eburnated bone.
Primary Osteochondrosis which leads to Osteochondritis Dissecans (OCD) can also occur, which is a failure of normal development of epiphyseal cartilage, usually affecting the medial aspect of the humeral condyle. Occasionally in certain breeds, ununited anconeal process (UAP) may occur, as may other forms of EI. In fact, Humeral Intercondylar Fissure (HIF) which commonly occurs in Spaniel breeds could also be considered a form of DED.
4. What individual characteristics are important to assess?
When discussing the options available to families of dogs affected by DED, it is vital that we can provide all of the options all of the time within one hospital facility. There are so many factors to consider when recommending treatment options including; the extent of the disease, the age of the patient, the impact on the patient’s quality of life, the wishes of the family, the varying level of risk involved in surgery, the financial situation of the family, the dog’s response to medication, plus many more!
5. When should I refer a patient?
A patient should be referred when medical management is deemed suboptimal or your client wishes to pursue alternative options such a surgery or comprehensive medical management such as regenerative medicine and rehabilitation. DED is inexorably progressive but early intervention can ameliorate disease and significantly improve quality of life.
6. Typically how long from referral do you see an orthopaedic case?
Our aim is to attend all routine orthopaedic cases within 1 week of referral and emergency orthopaedic referrals are usually seen on the same day. Patients with complex problems, previously seen by multiple referral centres may wait a little longer whilst we collate the imaging from other hospitals and work through the available information to allow us to give the best advice for each patient.
7. Does early intervention have a positive effect on prognosis?
In dogs affected by DED, the development and progression of osteoarthritis is inevitable. However, the pace at which that occurs is very variable and cannot be predicted. Therefore, we firmly believe that early referral can prove beneficial long-term. The objective is to accurately diagnose the specific form of DED and to explain all options available. This could vary from filling a focal defect in osteochrondritis dissecans (OCD) to focal arthroscopic debridement to unloading osteotomies. Early diagnosis and intervention is fundamental in our view.
8. What surgical treatment options are available?
Fitzpatrick Referrals offer more surgical options for DED than any other practice in the world. Treatment options can be largely split into surgical and medical management, though occasionally patients will benefit from a combination of both.
Surgical options for the management of DED and osteoarthritis are vast but largely depend on the stage of disease and age of the patient. From low-level to high-grade disease, options include; Biceps Ulnar Release Procedure (BURP), Distal Ulnar Osteotomy (DUO), Subtotal Coronoid Ostectomy (SCO), Bioblique Dynamic Proximal Ulnar Osteotomy (BODPUO), Proximal Abducting Ulnar Osteotomy (PAUL), Sliding Humeral Osteotomy (SHO), Canine Uni-Compartmental Elbow (CUE), Custom Medial Compartment Elbow Replacement (cMCR), Custom Total Elbow Replacement (cTER).
BURP and DUO can be performed in the very early stages of disease where a specific stress pattern is identified, which affects the coronoid process of the ulna. The stress arises from excessive and repeated forces imparted by a poor fit of the humero-ulnar joint. In selected cases, either cutting a segment out of the ulna or surgical release of the attachment of the biceps muscle on the coronoid process can reduce the forces acting within the badly fitting bone geometry and help slow further micro-fracture or fragmentation.
An SCO removes a fissured or fragmented portion of the coronoid process of the ulna and is usually performed arthroscopically. Cutting the ulna at an oblique angle and allowing it to heal in a more congruent position (BODPUO) can reduce the effect of poor fit of the elbow, relieve pain and potentially slow down progression of disease.
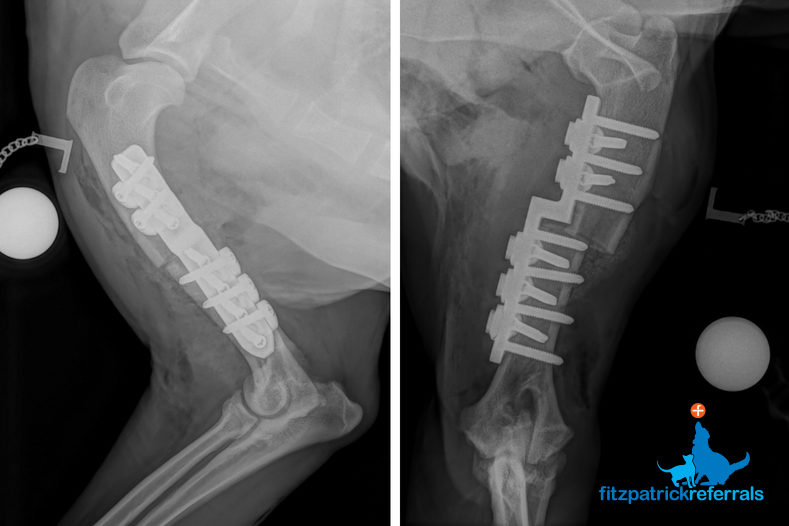
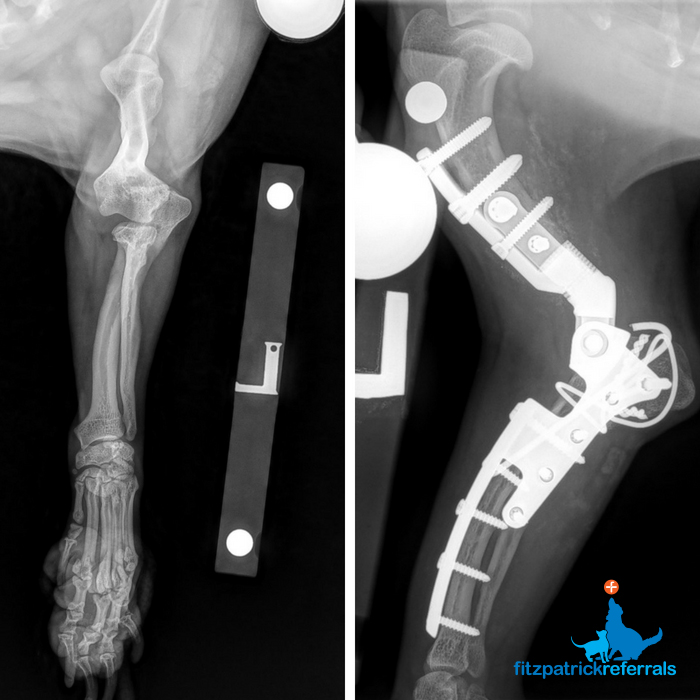
A PAUL involves cutting the ulna and securing it into a new position with a special plate and screws to unload the affected medial compartment of the elbow and drive force through the less affected lateral compartment, thus providing pain relief.
SHO is generally employed in young dogs with severe erosion of the medial compartment. A cut is made through the humerus, which is secured in a new position with a plate and screws. A custom-made SHO system has been developed and is successfully employed at Fitzpatrick Referrals. This allows more accurate unloading and more secure fixation.
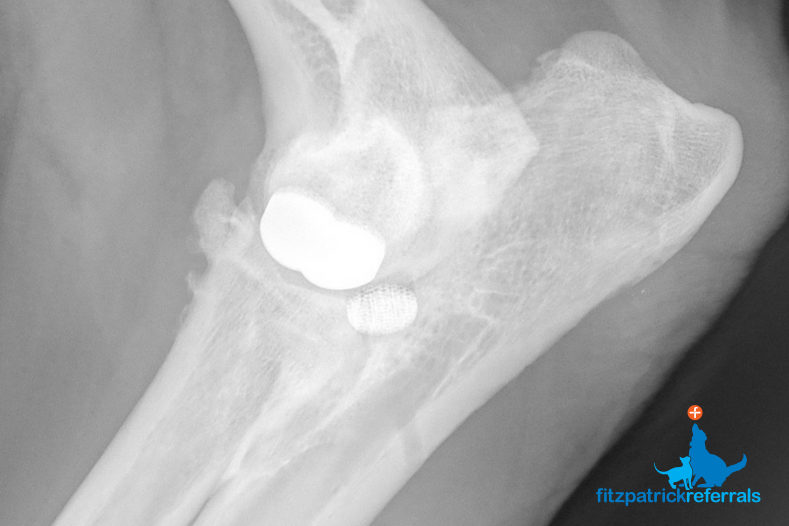
For treatment of Osteochondritis Dissecans (OCD) we can offer cSHO (with or without adjunctive injection of chondrogenically differentiated and anti-inflammatory stem cells) or implantation of a scaffold plug seeded with stem cells or implantation of a synthetic polycarbonate urethane implant with a trabecular metal backing (SynACART™). The latter two are generally accompanied by a BODPUO to reduce humero-ulnar conflict.
When the cartilage covering the medial compartment of the elbow is completely eroded and severely collapsed, but the radial head is intact, then the medial compartment can be resurfaced with metal and plastic components on the humeral and ulnar surfaces respectively.
A commercially available system (CUE) can be employed, but if cartilage erosion is deemed too extensive to benefit from these implants which have a relatively small surface area, then a Custom Medial Compartment Elbow Replacement (cMCR) can be employed to ensure as much joint surface coverage and as much pain relief as possible.
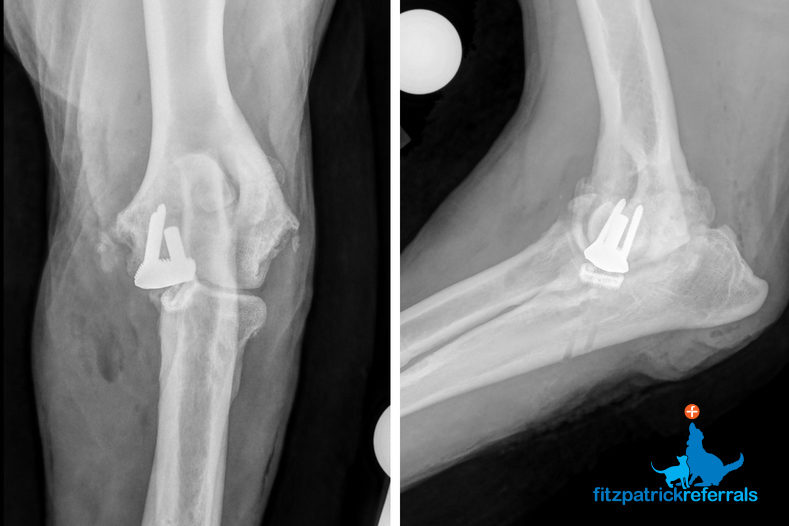
Where cartilage covering the medial and lateral compartments of the elbow (ulna and radius) is severely eroded, a Total Elbow Replacement (TER) may be indicated. Fitzpatrick Referrals has been working hard for a number of years to develop an effective custom TER system, as we have experienced challenges with commercially available systems. We currently offer custom Total Elbow Replacements (cTER) in a small number of patients following a comprehensive consultation with Professor Noel Fitzpatrick.

9. What medical treatment options are available?
Our Osteoarthritis Clinic is an innovative and comprehensive clinical service all under one roof, meaning your patients benefit from the support of our highly-specialised facilities, world-class specialists, dedicated rehabilitation service and extensive patient care team. The Osteoarthritis Clinic offers hour-long consultations, comprehensive medication protocols, physiotherapy, hydrotherapy and regenerative medicine options such as skeletal stem cells (SSCs) and platelet-rich plasma (PRP). The benefits of each option and the suitability for each patient is individually discussed in consultation.

Regenerative Medicine
10. What are skeletal stem cells (SSCs) and platelet-rich plasma (PRP) and what do they do?
SSCs are present in the tissues of mammals, and are equipped with the capacity to mediate inflammation, orchestrate wound repair and generate new tissue. They are multipotent, which means they can differentiate or develop from their stem cell state into cells of the skeletal system including bone, cartilage and connective tissue. These cells have a very well-known phenotype (or well-known characteristics) and have a known location within the body associated with small blood vessels (such as those within adipose tissue) and the lining of bone marrow cavities.
PRP is an autologous processed plasma product that contains supra-physiologic concentrations of platelets and growth factors. Administration of intra-articular PRP for treatment of cartilage injuries is thought to decrease inflammatory and degradative processes involved in osteoarthritis, provide analgesic effects, enhance joint lubrication, and potentially increase chondrocyte and stem cell proliferation.
11. What is involved if a client elects for regenerative medicine?
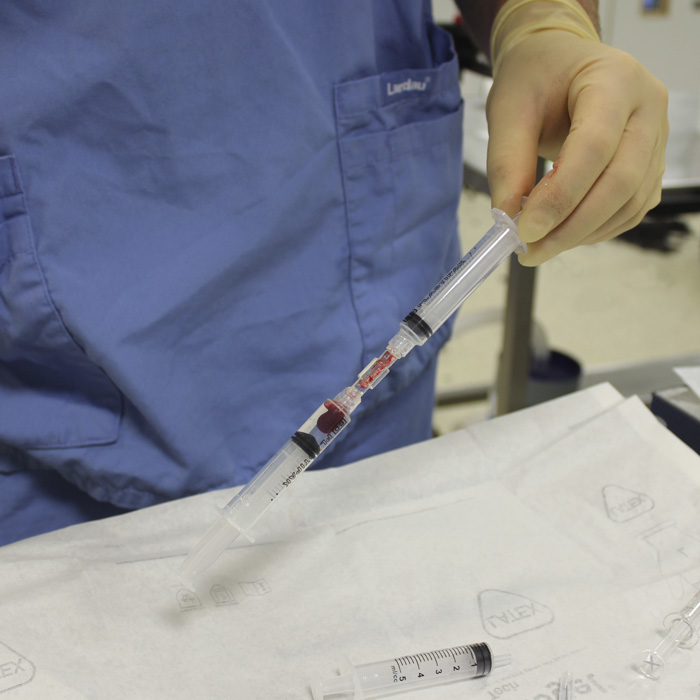
Patients will be booked in for a general anaesthetic and fat tissue harvest which will be taken from the lower abdomen. The cells will be isolated and grown from the fat and be ready 10-20 days later when they will be injected into the affected joint(s) under sedation. The specific elucidation and purification process we use is unique to Fitzpatrick Referrals, as is our combination of SSCs and PRP.
Comprehensive follow-up appointments are made to monitor and manage a patient’s response to therapy, including highly sensitive force-platform analysis of gait. Fat tissue and isolated cells will be stored, allowing repeated injections over time in patients who saw a good initial response, meaning that repeated general anaesthetic and fat harvest is not required.

12. What are the risks of skeletal stem cell therapy?
We use autologous stem cells and are simply re-injecting a purified population of regenerative cells harvested from the patient’s own tissue, and as such are highly unlikely to pose any risk. The process of taking tissue involves a general anaesthetic followed by a sedation when the cells are reinjected. Both of these do carry a small element of risk, the same as any other procedure carried out under anaesthetic. All our patients receive a comprehensive pre-operative health check to ensure they are healthy enough to undergo surgery.
Advice for your patients
We know that on occasion, speaking to one of our specialists is valuable and enables you to deliver the best options to your client. We are available every day to provide advice to vets and one of our orthopaedic clinicians will call you back within one hour of making a clinical enquiry.* Please call the Orthopaedics and Neurology practice on 01483 423761.
*Advice within 1 hour applies to normal working hours (8 am – 8 pm) Monday to Friday. We can give advice for emergency case out-of-hours.
Read our client page on developmental elbow disease
12 minute read
In this article






